- The Beat | Vasculearn Network
- Posts
- The Beat | June 2025
The Beat | June 2025
Patient Education by Vasculearn Network
Table of Contents
Building Momentum Together: Highlights from the VLN Board Retreat
There’s something powerful about being in the same room. This year’s VLN Board Retreat brought together dedicated leaders, passionate staff, and longtime supporters for a few energizing days of connection and collaboration in Sea Island, Georgia.

Top row left to right: Nathan Connell, John Fanikos, JoMarie Monzon, Brandon Linn, Christian Ruff, Tara Lech
Middle row left to right: Alfonso Tafur, Adam Judeh, Kathryn Mikkelsen, Margo Minissian, Joelle Hochman, Aviva Schwartz, Scott Woller.
Bottom row left to right: LaVon Woodard, Courtney Anderson, Jelena Spyropoulos, Courtney Battaglia, Heather Johnson
Throughout our time together, we reflected on what’s working, what’s needed, and what’s possible. The energy in the room made one thing clear: when we come together, we can make meaningful change.
Thanks to the ideas and momentum sparked at the retreat, we’re already moving forward. Our team is focused on making it easier to connect with others, access trustworthy information, and feel supported every step of the way.
To our community: we’re so glad you’re here. We’re building this with—and for—you. Here’s to what’s next.
Looking for support, connection, and trusted education?
1. Visit vln.thrombosis.org
2. Create a username and password.
3. Join the free, trusted online community.
4. Share your story with other patients and clinicians.
5. Visit often!
A Dismissed Diagnosis: LaVon’s Story
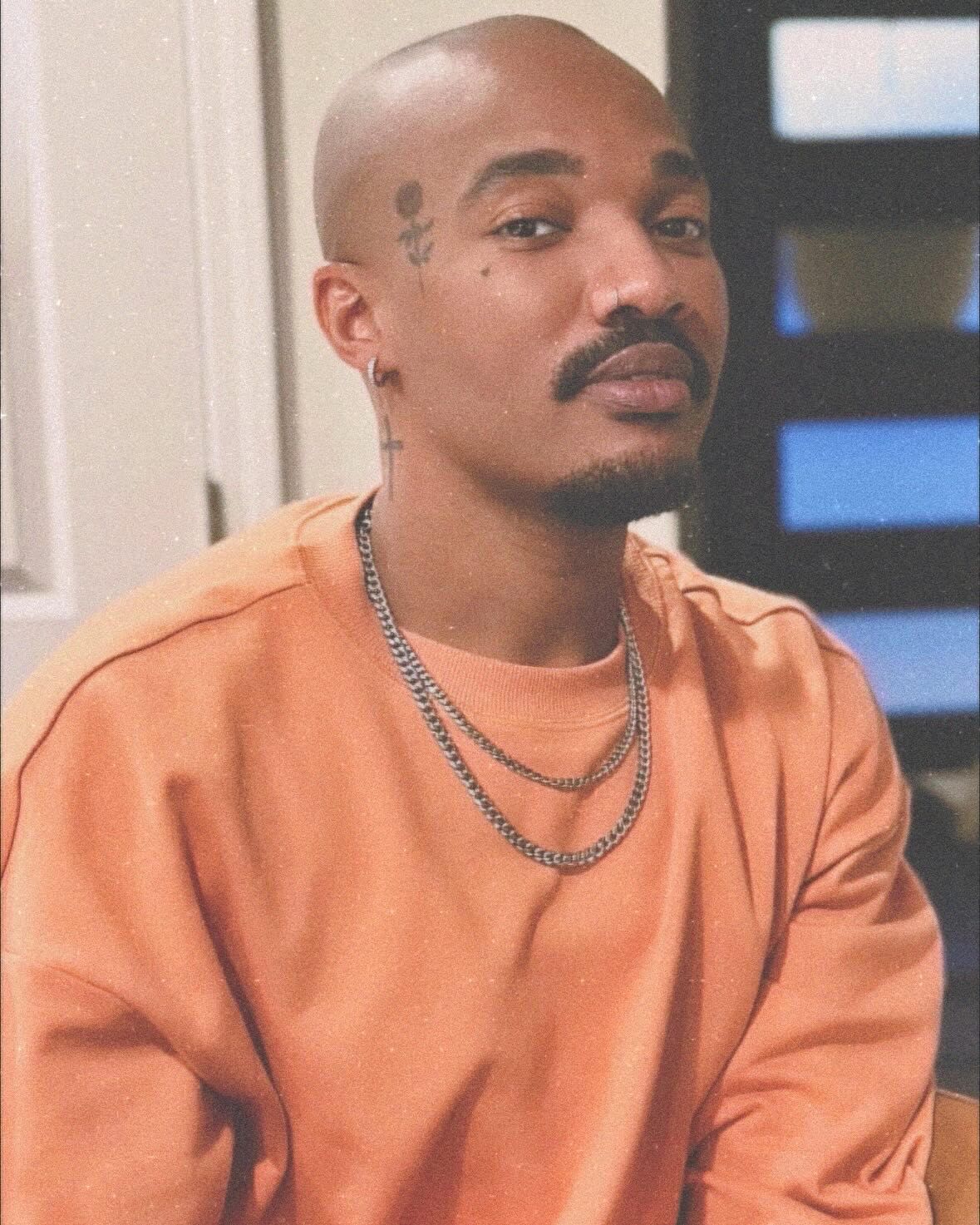 | In 2017, LaVon was at the gym when he felt sudden pain in his right leg. At first, he didn’t think much of it and went home. But the pain worsened, and his leg began to swell. He went to the emergency room and shared his family history of blood clots. “You look healthy, so I don’t think it’s a blood clot,” the doctor told him, recommending leg elevation and rest. A few days later, his primary care doctor said the same thing. |
For five years, LaVon lived with pain, swelling, and visible changes to the skin on his leg. It wasn’t until 2022 that he finally got the answers he needed. LaVon shares his experience, what he wishes he had known, and what he wants others to learn from his journey.
When did you first notice something was wrong?
At the gym, my leg suddenly started hurting. I thought maybe I’d pulled a muscle or something, so I went home to see if it’d go away. As the evening went on, my leg started swelling and the pain worsened. Even though this happened a while ago, I can still remember that pain. It felt like a bad bruise, almost like someone had kicked me in the leg. It was so painful that I could barely walk. I remember crawling to the restroom because putting weight on my leg hurt too much. That’s when I knew something was seriously wrong.
What else did you notice?
The swelling went from my ankle to my calf. My friends said my right leg looked different from my left. Over time, the hair on my leg fell out, and the skin got shiny and reddish.
How did you finally get diagnosed?
In 2022, I was getting ready to take a trip to Africa. I wanted to get my leg checked out before my trip and decided to switch doctors. I mentioned my leg pain and my family history of blood clots to my new doctor. She ordered an ultrasound and blood work. That's when I found out I had deep vein thrombosis (DVT) in my leg.
How did you feel when you got the diagnosis?
At first, I was terrified but also relieved to have an answer. I didn't know enough about blood clots before to know that I was going to be okay once I started treatment. I knew what could happen if a blood clot was left untreated and I was lucky that mine didn't turn into something more serious. I worried about moving too much because I thought the clot might travel. Once I talked to my doctor, I understood that staying active was important.
What was your treatment plan?
My doctor prescribed Eliquis® (apixaban), a blood thinner. At first, my doctor wasn't sure if I needed to go to the hospital, but then she decided I could start treatment at home. I'm still on blood thinners because of my family history of blood clots. My doctor also mentioned I may have Factor V Leiden (a genetic mutation that can increase the risk of clotting), but I haven't been tested for it yet.
What changes have you made to your daily routine?I stay hydrated and make sure to move throughout the day. I work as a barber, so I stand a lot. I take a few steps every 45 minutes to keep my circulation moving. I still work out. I also wear compression stockings, which help with swelling. I have to be extra careful at work because I use sharp tools like razors and shears. Since I'm on blood thinners, even a small cut can bleed more than usual. |  |
Do you still have the clot?
Yes, it's still there. I get ultrasounds twice a year. It hasn't gotten bigger, but it hasn't gone away either. The clot is just there. My hematologist reassured me that some clots take longer to dissolve, and as long as I keep taking medication, I’ll be fine. The pain’s gotten better. In fact, it was recently that I noticed the pain was starting to decrease.
What’s your advice to others with a new diagnosis?
Don't panic. Treatment works. Ask your doctor questions about what you can and cannot do. I wanted to know if I could still exercise and work long hours on my feet. Getting those answers made me feel more in control.
 | And for those who feel dismissed? Speak up. If a doctor dismisses your concerns, ask them to check again. You don’t have to be disrespectful but be firm. If you feel that you're not being heard, find a provider that will really listen. You must advocate for yourself.Speak up. |
Any final thoughts?
Know the signs of a blood clot. Pain, swelling, and redness are big warning signs. If I had known that earlier, I would’ve pushed harder. Don’t be afraid to speak up; it could save your life.
Men—Your Vascular Health Called. Time for a Checkup
Many men aren’t thinking about their vascular health—but problems can build long before symptoms appear. In honor of Men’s Health Month, we’re taking a closer look at vascular health: what it is, why men face earlier risks, and what you can do to protect yourself.

How Vascular Health Is the Common Link
The vascular system is made up of capillaries, arteries, and veins that work together to deliver oxygen and nutrients throughout your body. Vascular health refers to how well your blood vessels function—how flexible they are, how easily blood flows through them, and whether they’re free of blockages. Blood flows freely when your vessels are open and healthy, which reduces your risk of serious health problems. But when blood vessels become stiff, narrowed, or blocked, complications can occur.
Heart attacks
The arteries that deliver blood to your heart can become blocked by plaque—fatty deposits that build up inside the vessels. If the plaque ruptures, a clot can form and stop blood flow. When that happens, part of the heart muscle can become permanently damaged, leading to a heart attack.
Stroke
A stroke occurs when blood flow to the brain is disrupted, cutting off the oxygen that brain cells need. Strokes can be caused by a blocked vessel (ischemic stroke) or a rupture that leads to bleeding in the brain (hemorrhagic stroke).
Atrial fibrillation (AFib)AFib is an irregular heartbeat that affects how well the heart pumps blood. It often starts when there are changes in the upper chambers of the heart (the atria)— like scarring from a past heart attack, enlargement of the atria, or weakening of the muscle. These changes can disrupt the heart’s electrical signals, causing the atria to beat out of rhythm. When that happens, blood may pool and form clots. If a clot travels to the brain, it can cause a stroke. |  |
Why Men Are at Higher Risk
Men face heart-related conditions earlier in life than women. Men often have their first heart attack 6 to 10 years sooner than women, face strokes at younger ages, and are more likely to develop AFib.
Here’s the big question: why does it affect men more—and sooner?
Hypertension and high cholesterol occur earlier
High blood pressure often starts in men between the ages of 40 and 60. They also tend to have lower levels of nitric oxide, a compound that helps blood vessels relax and stay flexible. Without routine checks, high blood pressure may go unnoticed and silently damage the vascular system for years.
Men are also more likely to have high LDL (the “bad” cholesterol) at younger ages, which contributes to artery clogging plaque that can start as early as the teenage years. Estrogen helps regulate cholesterol levels, which may explain why women often have lower LDL levels until menopause.
Hormones and lifestyle habits play a role
Before menopause, estrogen helps protect women’s blood vessels by reducing inflammation, improving flexibility, and lowering plaque buildup. Men have higher testosterone levels, which may lead to more inflammation and unstable plaque that's more likely to rupture.
In some large studies, men were more likely to smoke, be less active, and skip checkups. Delayed screenings mean that warning signs can go unnoticed until something more serious occurs. These behaviors increase the risk of earlier disease.
How Men Can Lower Their Risk
Men can take simple steps to lower the risk of heart attacks, strokes, and afib. These changes matter—even if you start later in life.

Get regular checkups. Ask your doctor to check your blood pressure, cholesterol, and blood sugar at least every few years—more often if you're over 40 or have other risk factors.
Be active most days. Try to get 150 minutes of moderate activity (like brisk walking, biking, or swimming) each week. Short on time? Just 30 minutes a day, 5 days a week, can make a big difference.
Eat for your heart. Focus on fruits, vegetables, whole grains, fish, nuts, and lean proteins. Cut back on red meat, processed food, sugary drinks, and foods high in salt or trans fats.
Watch your weight. Extra weight, especially in the belly area, raises your risk for high blood pressure and AFib. Losing just 5 to 10 percent of your body weight can help improve how your heart and blood vessels function.
Quit smoking. Every tobacco-free day helps lower your risk of blood clots and other serious health problems. If you're ready to take the next step, smokefree.gov offers support and tools to help you get started.
Drink less alcohol (or none at all). Too much can raise your risk for AFib and stroke. It’s also linked to other serious health issues, including some cancers, especially in older adults.
Manage stress. Long-term stress raises blood pressure and increases inflammation. Daily walks, deep breathing, and getting enough sleep can help.
Take sleep problems seriously. Loud snoring, gasping during sleep, or always feeling tired could be signs of sleep apnea, which is linked to high blood pressure and AFib. It’s treatable—so bring it up at your next checkup.
You don’t have to change everything at once. Pick one or two areas to start with and build from there. Many men start making changes in midlife (around ages 40 to 65) or beyond and still see major benefits.
Meet our newest team member, Courtney
 | Hi! I’m Courtney, the new Patient Education & Community Content Manager at VLN—and the writer behind The Beat, our newsletter. I live in the scenic Texas Hill Country and bring 16 years of experience as a registered nurse. Throughout my career, I’ve worked in a wide range of specialties, from cardiovascular care to autoimmune disorders and oncology. One thing that’s always stayed the same? My love of patient education. Hi! I’m Courtney, the new Patient Education & Community Content Manager at VLN—and the writer behind The Beat, our newsletter. |
I live in the scenic Texas Hill Country and bring 16 years of experience as a registered nurse. Throughout my career, I’ve worked in a wide range of specialties, from cardiovascular care to autoimmune disorders and oncology. One thing that’s always stayed the same? My love of patient education. I also love writing, which led me into health communication. I’m passionate about making medical information easier to understand and grounded in science. I believe education can be empowering, and am honored to support this community by helping share stories, resources, and tools for healing.
Outside of work, I’m a self-taught (and still learning!) home cook. I bake a lot— Carmelita bars are my go-to—and I’m usually balancing cooking and writing with a full family life. If there’s a topic you’d like to see covered or something on your mind, I’d love to hear from you. Reach out in the community anytime!
Upcoming Patient Events
Blood Clot Support Group
Hosted by Joelle Hochman, RRT, Chair of Patient Engagement & Education After experiencing a blood clot, it’s normal to have a lot of questions. Many people are left feeling confused about why this happened to them and are anxious about it happening again. |  |
We’re pleased to offer a support group experience where patients can share their stories, connect with others who’ve had blood clots, and receive emotional support.
June 17, 2025
July 17, 2025
August 21, 2025
September 18, 2025
Spanish-speaking Support Group
 | We’re excited to offer a virtual support group series for Spanish speakers. Led by expert physicians, these sessions provide practical guidance on heart health in a supportive, interactive space. |
Participants can join live Q&As and discussions tailored to their needs.
June 18, 2025
Ask the Experts
Our Ask the Expert series, formerly called Blood Clot Education Group, is a space to connect with others and learn about all things related to blood clots and overall vascular health. |  |
Get accurate information on the latest research and treatments, and share your experiences.
July 15, 2025
August 12, 2025
In all online groups, a clinician will be available to answer general questions. Please note that they cannot provide personalized medical advice to any patients.
Do you like what you see in The Beat and find this information helpful? Please consider making a small donation to VLN to further support blood clot education.
References:
Acute myocardial infarction - The New England Journal of Medicine
Association of Younger vs Older Ages With Changes in Incidence of Stroke and Other Vascular Events, 2002-2018 - JAMA Network
Diverging Trends in Age at First Myocardial Infarction: Evidence from Two German Population-Based Studies - Scientific Reports
Sex differences in endothelial function important to vascular health and overall cardiovascular disease risk across the lifespan - American Journal of Physiology-Heart and Circulatory Physiology
Sex differences in risk factors for myocardial infarction: cohort study of UK Biobank participants - The BMJ
Vascular Diseases - MedlinePlus
What is Atrial Fibrillation - American Heart Association
2021 ACC Expert Consensus Decision Pathway on the Management of ASCVD Risk Reduction in Patients With Persistent Hypertriglyceridemia: A Report of the American College of Cardiology Solution Set Oversight Committee - Journal of the American College of Cardiology
|

Reply