- The Beat | Vasculearn Network
- Posts
- The Beat | February 2025
The Beat | February 2025
Patient Education by Vasculearn Network

Table of Contents
Goodbyes and Hellos: Meet the 2025 Medical Advisory Board
The Medical Advisory Board (MAB) was founded in 2020 to support the North American Thrombosis Forum (NATF – now Vasculearn Network, VLN) in delivering timely, relevant educational resources to both clinicians and patients. Over the past four years, the MAB has not only guided us through a global pandemic but also played a pivotal role in shaping our mission, vision, and strategic goals.
We wouldn’t be the organization we are today without the dedication, expertise, and passion of this incredible group of advisors. To our emeriti members: thank you for your invaluable contributions. We deeply appreciate your time, knowledge, and commitment.
Though these departures are bittersweet, we’re thrilled to welcome new perspectives and leadership in 2025. Members of the VLN Medical Advisory Board (MAB) will serve as both advisors to—and advocates for—the organization and will focus on:
Offering insights, scientific guidance, and expertise to advance VLN’s mission
Enhancing our visibility
Supporting our strategic growth and development
💜 A heartfelt thank you to our outgoing members:
Aaron Aday, MD, MS
Allen Taylor, MD
Alex Spyropoulos, MD
Brenda Shisslak
Jerrold Levy, MD
Margaret Fang, MD, MPH
Umberto Campia, MD, MSc
The 2025 VLN Medical Advisory Board
Behnood Bikdeli, MD, MS
Vascular Medicine Advisor
Heather Johnson, MD, MS
Preventive Cardiology Advisor
JoMarie Monzon, FNP-BC, MSN
Vascular Surgery / Advanced Practice Provider (APP) Advisor
LaVon Woodard
Patient Advisor
Margo Minissian, PhD, ACNP
Technology & Innovation Advisor
Scott Woller, MD
Thrombosis Medicine Advisor
Taylor Anzidei, DNP-EL, RN, CCRN
Clinical Nursing Advisor
Introducing our Newest Medical Advisory Board Members
 Heather Johnson, MD, MS | Dr. Heather M. Johnson is the Director of Preventive Cardiology for Women’s Services at Florida Atlantic University. She earned her medical and population health degrees from the University of Wisconsin-Madison and a Master of Medical Management from USC. Her NIH-funded research focuses on cardiovascular risk management, and she is a Fellow of multiple cardiology organizations. |
JoMarie, Lead Nurse Practitioner for the Division of Vascular Surgery at Cedars-Sinai Medical Center, oversees advanced practice initiatives and protocol development. A Nurse Practitioner since 2009 with board certification, she has led projects like an APP-led aortic clinic and expanding vascular surgery services. JoMarie was named Cedars-Sinai APP of the Year (2023) and is developing a sclerotherapy clinic for venous disease. |  Jomarie Monzon, FNP-BC, MSN |
 LaVon Woodard | LaVon Woodard, a licensed barber and barbershop owner in Brunswick, Georgia, experienced symptoms of a leg blood clot in 2017 but was sent home without treatment. In 2022, he was diagnosed with deep vein thrombosis (DVT). He is grateful to be a part of the VLN Medical Advisory Board, where he can share his story and learn from Vasculearn Network. |
LCDR Taylor Anzidei is a critical care nurse and leader in the U.S. Navy Nurse Corps. She specializes in trauma and cardiovascular care, advanced cardiac devices, and military medical readiness. Taylor is a decorated officer, educator, and speaker, committed to advancing military healthcare and mentoring the next generation of nurses. |  Lieutenant Commander Taylor Anzidei |
 Scott Woller, MD | Dr. Woller, a specialist in thrombosis medicine and anticoagulation, focuses on venous thromboembolic disease prevention. A Professor of Medicine at the University of Utah and Chair of Medicine at Intermountain Medical Center, he has led NIH-funded studies and co-chaired ACCP antithrombotic therapy guidelines. Board certified in Internal Medicine, Dr. Woller is a Fellow of major medical societies and a renowned educator. |
We are also pleased to announce that Tara Lech and Aviva Schwartz will continue to co-chair the Board for the 2025 term, and Behnood Bikdeli and Margo Minissian will stay on for their second term. We look forward to exciting collaborations ahead as we remain committed to advancing cardiovascular and thrombosis education and improving patient care.
Heart Failure’s Quiet Companion: The Risk of Blood Clots
Heart failure (HF) is a serious condition that affects millions of people worldwide and is becoming more common as the population ages. Most people know that it causes fatigue, swelling, and shortness of breath. Few realize that the condition also increases the risk of blood clots.
Raising awareness about this connection is one step forward in improving outcomes for those living with heart failure.
What Is Heart Failure?
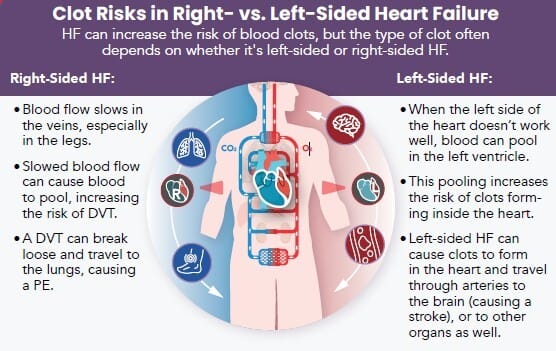
HF occurs when the heart has trouble pumping properly. The walls of the heart might be stiff or damaged, or the heart muscle might not pump as strongly as it should. These problems can raise pressure in the heart or reduce its ability to circulate enough blood to support the body, whether at rest or during activity. HF can affect different parts of the heart, resulting in:
Left-Sided HF: The left side of the heart pumps oxygen- rich blood to the body. When it doesn’t work properly, fluid may build up in the lungs, and make breathing difficult. This can be described as systolic HF (trouble pumping blood out) or diastolic HF (the pumping chamber becomes stiff, doesn't relax between beats, making it harder to fill with blood).
Right-Sided HF: The right side of the heart sends blood to the lungs to pick up oxygen. When this side fails, blood backs up in the veins, causing swelling in the legs, ankles, or belly.
Understanding Blood Clots
As part of the body's natural healing process, blood clots form when a blood vessel has become damaged. Platelets and proteins in the blood work together to create a clot that stops bleeding and protects the injured area. Sometimes, clots can form inside blood vessels even when there's no clear injury, or they may not break down as they should, leading to serious health risks.
Why Does Heart Failure Increase Blood Clot Risk?
HF raises the risk of blood clots in several ways, including slowing blood flow and damaging blood vessels. These changes create conditions where dangerous clots, like deep vein thrombosis (DVT) or pulmonary embolism (PE), are more likely to form.
Damage to blood vessel walls
Heart failure can damage the walls of blood vessels, leading to endothelial dysfunction, a condition where the vessel lining loses its ability to work properly. Increased pressure in the vessels, abnormal blood flow, and oxidative stress—an imbalance of harmful molecules that damages the vessel lining—are key contributors. Over time, this damage weakens the vessels' ability to relax and regulate blood flow.
Changes in the blood
Inflammation in HF raises levels of clot-promoting molecules like fibrinogen. It also activates platelets, making them stickier and more likely to form clots. Oxidative stress disrupts the blood's natural balance between clotting and anti-clotting factors. Medications used to reduce fluid buildup in HF can increase blood concentration and further promote clot formation.
Altered blood flow
When HF reduces the heart’s pumping ability, it can lead to low cardiac output, where less blood is pumped out than normal. Over time, the heart’s chambers may stretch and enlarge, further weakening its function. This slower blood flow increases the risk of blood clots. Atrial fibrillation (Afib), a common condition in people with HF, can further disrupt blood flow.
In Afib, the heart's irregular rhythm causes blood to pool in the atria, the two chambers of the heart that receive blood and pump it into the ventricles. This pooling creates an environment where clots are more likely to form. These clots can travel to the brain, leading to a stroke.
Living Well with Heart Failure and Blood Clot Risks
Take your medications as prescribed and follow your clinician's advice for managing other conditions that can make HF worse. Follow these tips to help manage HF and reduce your risk of blood clots:
Stay physically active: Regular movement improves heart health and prevents blood from pooling.
Stop smoking: Smoking increases your heart rate and blood pressure and reduces your ability to stay physically active.
Get enough rest: Take breaks to reduce strain on your heart. Simple things like napping, putting your feet up, or sitting during tasks can prevent overexertion. For better sleep, avoid caffeine, alcohol, and heavy meals before bed.
Manage stress: Use healthy coping methods like deep breathing, yoga, or joining a support group.
Eat heart-healthy foods: Focus on fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit processed foods, sugar, salt, and red meat.

HF can lead to blood clots, but understanding the connection can help you take control. Small, consistent steps—like following your care plan and addressing risk factors—can make a big difference in protecting your health.
Upcoming Patient Events
Blood Clot Education Group

Join our Blood Clot Education Group to connect with others and learn about all things related to blood clots. Get accurate information, hear from experts on the latest research and treatments, and share your experiences. Each session includes participant introductions and a Q&A with a clinician, where you can submit questions in advance.
Hosted by Joelle Hochman, RRT, Chair of Patient Engagement & Education. After experiencing a blood clot, it’s normal to have a lot of questions.
Many people are left feeling confused about why this happened to them and are anxious about it happening again.
Do you like what you see in The Beat and find this information helpful? Please consider making a small donation to VLN to further support blood clot education.
References
Atrial Fibrillation and Heart Failure – Journal of Clinical Medicine
Blood Clots – American Society of Hematology
Blood Clots – MedlinePlus
Blood Coagulation Disorders in Heart Failure: From Basic Science to Clinical Perspectives – Journal of Cardiac Failure
Impact of Atrial Fibrillation in Patients with Heart Failure and Reduced, Mid-Range or Preserved Ejection Fraction - Heart
Lifestyle Changes for Heart Failure – American Heart Association
Oxidative Stress and Inflammation in the Evolution of Heart Failure: From Pathophysiology to Therapeutic Strategies – European Journal of Preventive Cardiology
Stroke – Mayo Clinic
Types of Heart Failure - American Heart Association
|

Reply